Should you wear a face mask when you leave your house? It’s the question no one seems to agree on.
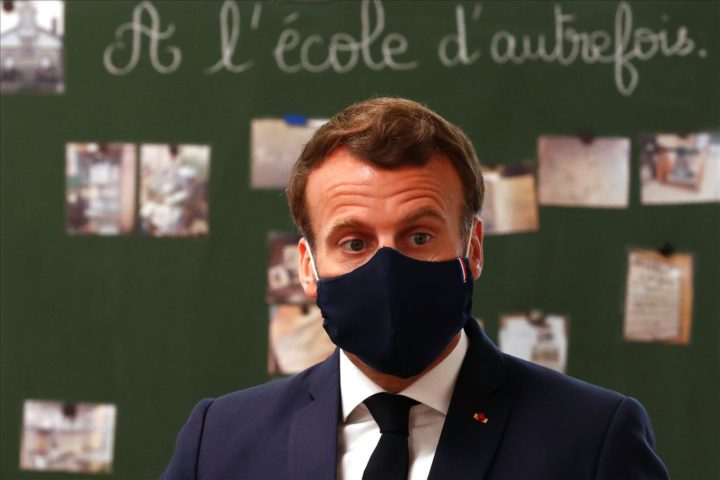
In France, the government originally said masks were unnecessary, but this week has made it mandatory to wear them on public transport and in secondary schools and is distributing masks through supermarkets and pharmacies. The UK government says it is still considering evidence on mask-wearing and is holding out on a recommendation, yet Scotland has already recommended that people cover their faces when in public spaces.
Meanwhile, in Michigan, a security guard has been shot and killed in a dispute over a requirement to wear a mask inside a store.
For its part, the World Health Organization (WHO) has not recommended the use of masks for healthy members of the public unless they are taking care of a COVID-19 patient.
This conflict in public health advice is confusing for the public. Why are some governments and agencies willing to recommend mask use when others aren’t, and why are recommendations changing?
At the heart of this confusion is the tension between two critical public health principles which agencies around the world are struggling to balance: the principle of effectiveness, and the precautionary principle.
The principle of effectiveness
The core value that any public health organisation adheres to is to do no harm to the people they have a responsibility to protect. If a community is at risk, the government may have a duty to recommend interventions, as long as those interventions will cause no harm, or are the least harmful option.
If an agency follows the principle of effectiveness, it will only recommend an intervention that they know to be effective. The problem is we do not yet know, for sure, whether wearing a mask will provide any benefits. Could it even cause harm? Will wearing masks result in people engaging in more risky behaviours – for example, socialising while wearing a mask, or reducing regular hand washing – in the belief that they are protected?

This is why the WHO has not recommended that members of the public wear masks, stating: “Currently there is not enough evidence for or against the use of masks (medical or other) for healthy individuals in the wider community.”
In this, it is adhering strictly to the principle of effectiveness, and always has done. The UK government and Public Health England are clearly also reluctant to move away from this principle.
The precautionary principle
So why are some governments recommending mask-wearing? It is likely because of the second principle organisations use when deciding whether to recommend an intervention – the precautionary principle.
In public health, the precautionary principle suggests that, if a possible threat to human health arises, we should take steps to manage that threat, even partially.
Using this principle, an agency will recommend an intervention when there is limited evidence of efficacy – that is, when the conditions of the principle of effectiveness are not met – given the nature of the threat to health. The idea, in this case, is that doing something might be better than doing nothing.
This principle has been applied by some humanitarian and public health agencies in response to air pollution crises, for example during volcanic eruptions and wildfires. In these circumstances, there is also limited evidence of mask efficacy for community use.
Nicola Sturgeon, the first minister of Scotland, has acknowledged that evidence of face mask efficacy is indeed limited, but she has said that there may be “some benefit in wearing a face covering if you enter an enclosed space where you will come into contract with multiple people and safe social distancing is difficult”.
The UK government is under significant pressure to follow suit. Sadiq Khan, the mayor of London, has called for compulsory public face mask use and, every day, the media are questioning why the UK government has not decided to recommend community use of face masks – it may seem a no-brainer to try a cheap intervention that appears, in some countries like Vietnam and South Korea, to have assisted in controlling the pandemic.
Equitable allocation
In addition to the ethical arguments around the principles of effectiveness and precaution, there is also the question of whether, in making a recommendation that everyone should wear masks, it is possible that those who require them the most will no longer be able to source sufficient supplies. There is a particular concern that healthcare providers and essential industries may not be able to procure personal protective equipment (PPE) for their staff.
So, if the UK government or the WHO does mandate, or recommend, that the public should wear face masks, we may expect this advice to include the use of homemade face coverings rather than medical-grade masks, in order to preserve stocks of PPE. Yet, there have been even fewer studies conducted on the effectiveness of cloth materials in reducing community transmission of viruses, than for PPE-quality masks.
There are good arguments in favour of both ethical principles, assuming there is not a supply issue. Recommending that members of the public take precautions by wearing a face covering may give the public a sense of reassurance, but we would argue that any recommendation should be accompanied by public information on the potentially limited efficacy of these interventions, and on the importance of continuing with social distancing and hand washing.
The mask-wearing problem is part of the same dilemma that has bedevilled most public health decision making throughout this pandemic. We do not have enough evidence to be able to make a definitive call on what works and what doesn’t. In the end, it may be public pressure, rather than new evidence, that causes the UK government to shift its position on whether people should wear masks.