According to the Centers for Disease Control and Prevention (CDC), an estimated 19 million Americans have been infected with the flu so far this season, and 180,000 of them have been hospitalized because of the illness. The flu virus has already killed an estimated 10,000 people across the U.S., including 68 children, according to the CDC.
Fourteen influenza-associated pediatric deaths occurring during the 2019-2020 season between weeks 45 and 4 (the weeks ending November 9, 2019 and January 25, 2020) were reported to CDC during week 4. Eight were associated with influenza B viruses; one had a lineage determined and was a B/Victoria virus. Six were associated with influenza A viruses, and three were subtyped; all were A(H1N1)pdm09 viruses. (Weekly U.S. Influenza Surveillance Report, Key Updates for Week 4, ending January 25, 2020)
Of the 68 influenza-associated pediatric deaths occurring during the 2019-2020 season and reported to CDC:
- 45 deaths were associated with influenza B viruses, and eight had a lineage determined; all were B/Victoria viruses.
- 23 deaths were associated with influenza A viruses, and 13 were subtyped; all were A(H1N1)pdm09 viruses.
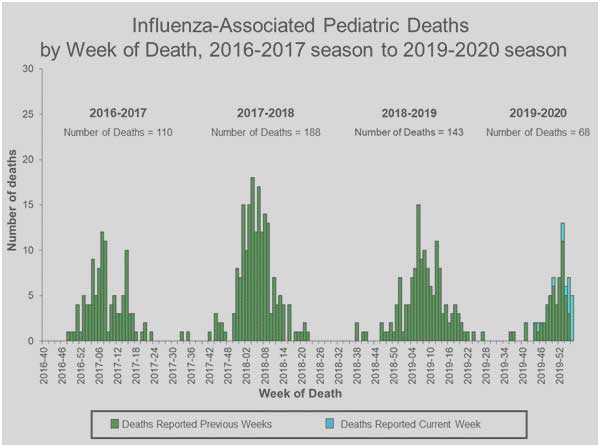
The 2019-2020 flu season has been particularly harmful to children. In mid-December, the CDC reported that six children had died from the flu. But the latest CDC statistics show that number has climbed to 27 children.
“Children are particularly vulnerable because their immune systems are not fully developed,” Randell Wexler, MD, a family medicine physician at The Ohio State University Wexner Medical Center, tells Yahoo Lifestyle. “In addition, children with asthma — as well as other chronic diseases — are more susceptible, and they do not respond to a viral insult the same way adults do. Children under the age of five in general, and those less than one year of age in particular, are most at risk.”
In contrast to this Flu situation in the U.S., the Wuhan coronavirus has infected more than 28,000 people and killed 565, according to data gathered by the John Hopkins University — though those numbers continue to rise.
Iahn Gonsenhauser, MD, chief quality and patient safety officer at Ohio State University Wexner Medical Center, said: “Flu is by far the thing we should be worried about because it’s the thing we’re more likely to encounter. If you’re a child, elderly, frail, or have COPD or heart failure, your risk of mortality is actually pretty high with the flu. Your risk of coronavirus — it’s 12 cases in the U.S. — you’re pretty unlikely to come into contact with them.”
One of the reasons why coronavirus is garnering much more attention than the flu has to do with how we process language — and in particular, medical terminology, Gonsenhauser explains. “We throw around the word pandemic — that terrifies people,” he says, noting the word can bring up the terrible pandemics from history, such as the bubonic plague and smallpox. “But really all we mean by that word is something that’s spreading across a large geographic area in a short amount of time. But it doesn’t necessarily indicate the virulence and deadliness of it. I think people think it’s like the movie Outbreak.”
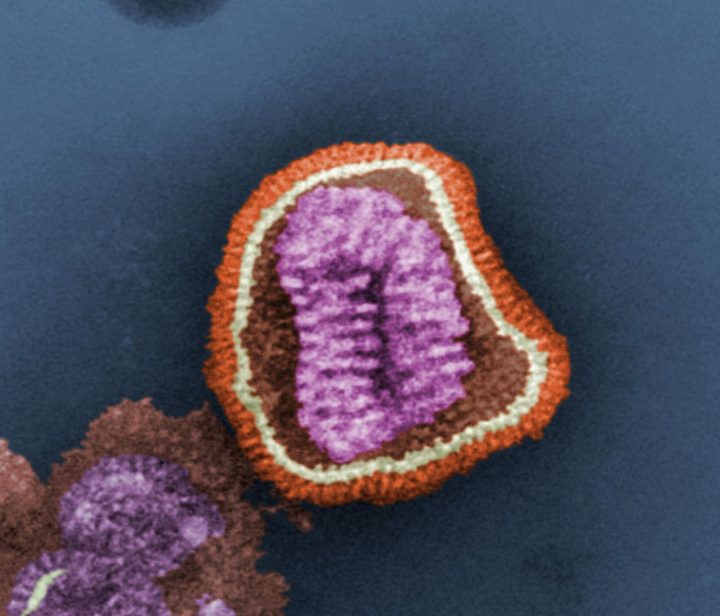
While coronaviruses are not new, this particular one (known as 2019-nCoV) is. “We’ve seen coronavirus before, but this is a new version,” Gonsenhauser says. “So any time there’s something new people automatically go to Ebola and the zombie apocalypse, thinking that it’s untreatable and deadly. That is not what we are seeing. It’s certainly spreading more rapidly than SARS did, but it’s not more dangerous than other viral strains.”
One factor that may be contributing to the fear surrounding coronavirus is that it shares similar symptoms with the flu, such as fever and cough, making it harder to tell what the disease the person coughing next to you on the train has. “The symptoms definitely overlap,” says Gonsenhauser. “One of the reasons that drives some of the panic is that this is happening during flu season. But if this were happening in the middle of summer when people weren’t getting colds and flu, it would be a lot more clear when people are coming back with symptoms we should be concerned about.”
In the meantime, Gonsenhauser stresses the importance of getting the influenza vaccine and practicing good hand hygiene. Even though we are well into flu season, he says, “It’s never too late to get a flu shot. Get one.”
Also, wash your hands with soap and warm or cold water for 20 seconds frequently throughout the day, and avoid touching your eyes, nose and mouth.
Gonsenhauser explains that the primary mode of transmission for viruses like the flu and coronavirus is person-to-person and through body fluids, such as saliva and mucus. “You think about the number of people who wipe their nose on the back of their hand and then touch a doorknob or escalator handle, and then you touch it moments later,” he says. “[Viruses] can live long enough to transmit that way.”
He adds: “If people were as concerned about influenza as they were about coronavirus we could potentially really create a much lower propensity for flu virus to spread in the U.S.”